The healthcare industry includes a complex work structure and critical responsibilities like patient care and recovery. Therefore, smooth information exchange is a crucial requirement in clinical services. Daily, vast amounts of data are exchanged between healthcare providers, pharmacies, patients, and laboratories. Patient documentation starts from admissions to insurance claims. In such a sensitive medical environment, even a little error in the information flow or a minor delay can lead to severe outcomes. Here, EDI Automation plays a significant role in the high-risk data exchange.
Electronic data interchange streamlines the digital transformation of the healthcare sector. EDI Automation in Healthcare electronically transfers standardized medical documents, including lab results or insurance claims. Hospitals and other care units can quickly and accurately share patients’ required information using digital services without manual intervention.
Table of Contents
What is EDI Automation in Healthcare and Why Does It Matter?
EDI Automation in Healthcare refers to the electronic data exchange of medical documents between medical service providing participants such as hospitals, labs, pharmacies, and insurance providers. The electronic system connects all the relevant clinical units and ensures fast and error-free communication, enabling a seamless transaction flow over the network. Digital workflow allows for the intelligent inventory management and timely delivery of medical products, pivotal for patient well-being. Regular records like patient eligibility checks, benefits enrollment, prescription fulfillment, and claims processing occur in the sector, and managing them manually is not feasible. EDI automates the whole transaction with the minimum requirement of human intervention and better performance. From the following key point, we can understand its importance:
- Effective integration of the digital tool helps reduce stock problems like shortages or wastage of injections, medicines, and medical equipment, which is prominent in avoiding mishappenings in healthcare.
- Current medical organizations face administrative overheads and pressure from the authorities to provide better patient outcomes with improved functional systems, which traditional paper-based methods can not attain.
- Automation has become necessary for eliminating compliance issues. And ensure compliance with regulatory measures such as HIPAA and avoiding regulatory risks related to patient personal data security.
In short, by adopting electronic methods for document exchange in the health industry, care providers can redirect their focus from transaction handling to nursing patients. Moreover, organizations aiming for competitiveness in the clinical sector should see EDI as a strategic need in the digital world rather than just a backend addition.
EDI Automation: Statistical Insights
Modern healthcare entities are seeking automation as a crucial component of information exchange. Data-driven insights listed below will help in understanding the importance and impact of EDI services in the well-being industry:
- CAQH 2020 Index reported that the healthcare industry can save up to $16.3 billion annually by implementing automated transactions in administrative tasks.
- Fully computerised complex processes cost approximately 42% less than using manual or partially digital portals in the US health sector.
- Medical organizations adopting automation for their revenue cycle management (RCM) report a 15%-20% labor cost reduction with improved accuracy.
- An electronic system speeds up the patient eligibility check and approval process, which used to take 21 days in manual processing, but with automation, it is done in a few hours, quickening the treatment decision.
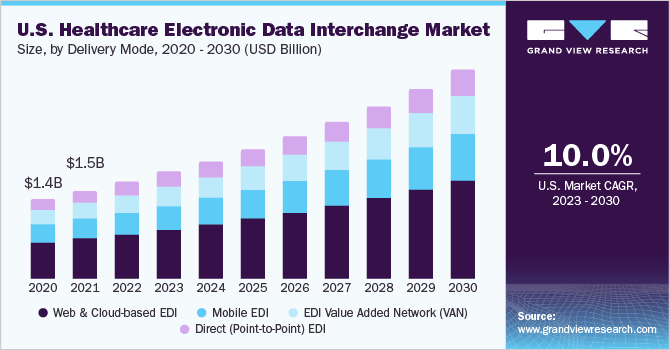
- The market size of EDI in global healthcare in 2022 was USD 4.41 billion and is expected to grow from 2023 to 2030 at a CAGR of 9.6%.
The above image shows the market size of different EDI types used in the US healthcare industry from 2020 to 2021 and anticipates a 10% US market CAGR until 2030 for the whole period starting from 2023.
How Does EDI Work in Healthcare Data Exchange?
Electronic data interchange promotes the systematic exchange of medical documents using HL7 or X12, structured formats, which automates the information processing on the recipients’ systems without reentering the particulars. Activities like claims submission, eligibility verification, and payment execution are much easier with streamlined communication and reduced errors. Let’s understand how EDI automation services work in healthcare data exchange in simple steps:
Data Preparation
The medical team enters the patient’s details, lab results, eligibility enquiry, or claims in their internal platform.
Translation
The system accordingly translates the entered data into appropriate and structured EDI records like 835 or 837.
Transmission
Translated electronic documents are then transmitted to the relevant parties, such as an insurance company or a pharmacy, through a secure protocol (e.g., FTP, VAN, or AS2).
Validation and Processing
The recipient of the data validates it for accuracy and compliance with the predefined standards. Once the validation is completed, the receiver’s system processes transactions such as generating payments or updating records.
Acknowledgment & Response
Upon processing, the recipient/payer responds to the sender by confirming the requested task’s initiation or rejection.
Hence, EDI automation services save time and resources for healthcare organizations by eliminating the wait for a course of action and speeding up the transaction cycle.
Real-World Use Cases of EDI Automation in Healthcare Organizations
Practical application of the digital transaction platform accelerates the operational efficiency of the medical units by optimizing their wide range of tasks chain. Actual uses of EDI Automation in Healthcare are:
Hospital Admissions and Discharges
A complete summary of the patient, starting from the point of admission to his discharge from the hospital, is conveniently transmitted to the relevant medical team and insurance company with the help of EDI. Digital exchange of data makes the claim settlement and accurate care billing effortless.
Referral Management and Lab Orders
Electronic systems provide consistent directing of referrals to specialists, based on patient medical records, and enable forwarding the lab orders, making it a rapid, error-free, and paperless process. Digital transmission of data establishes coordination between different caregivers and offers them access to accurate information about the patient’s health status.
E-prescriptions and Pharmacy Coordination
Smart transaction solutions put an end to wrong medication risks arising from misinterpretation of verbal orders and handwritten prescriptions. Also, the pharmacy receives clinical suggestions in real time via an electronic system, reducing delay and coordinating benefits that fasten the recovery time.
Insurance Pre-Authorizations and Claim Submissions
Structured data systems quicken the insurance claim submission and processing, using formats like 837, ensuring a speedy approval and reimbursement cycle. A lot of paperwork requirements are removed while improving cash flow in the health organization, which accelerates their financial status.
Medical Equipment Ordering and Inventory Management
EDI in healthcare optimizes its supply chain by connecting the supplier of the medical equipment with the hospitals, pharmacies, and labs. It reduces the risks of stockout and overstocking, facilitating inventory management of clinical machinery using electronic transactions.
Electronic Remittance Advice (ERA) Processing
Documents like 835 support the integration of automated remittance details in the accounting system, which helps in calculating final settlement with the patient or insurance provider, without the need for manual reconciliation.
Automated Enrollment and Disenrollment
During open entry season, organizations can manage benefits enrollment and disenrollment efficiently with minimum errors. Hospitals can easily put the names of new eligible patients in the health plans using the 834 file format.
Electronic Referral Submission and Tracking
EDI enables the swift movement of patient referral information between the care units, simplifying their access to the specialists’ services. It establishes coordination among the providers and helps them track Referral Submission in real time.
Automated Transmission of Lab Results
Lab results are digitally transferred into the electronic medical records, informing about the patients’ physical health. It enables physicians to make timely decisions regarding treatment and medication courses.
Secure Electronic Exchange of Patient Information
Automated exchange of documents under EDI ensures compliance with the HIPAA standards, securing the patient’s sensitive data transmission and reducing risks of breaches, while maintaining information privacy.

Top Benefits of Using EDI Automation in Healthcare Workflows
In the current healthcare scenario, multiple medical practices rely on EDI automation due to its advantages. To better understand the perks available through an electronic system, the following benefits provide better insights in this direction:
Speed and Efficiency
Electronic document interchange eliminates manual data processes, boosting accuracy and fast transaction speed. It reduces the work pressure of the medical staff and allows them to focus on nursing and care. Health organizations can improve their operational efficiency for tasks such as managing eligibility, claim processing, and payment handling. All these activities used to take a lot of time with traditional methods; however, EDI automation in healthcare helps to perform these tasks within minutes.
Cost Savings
With the elimination of physical data entry and paper-based documentation, managers can reduce costs like administrative overheads, paper expenses, and labor charges. Also, electronic platforms significantly minimize the time consumed by major tasks in hospitals like claim processing, checking insurance eligibility, and billing. Staff can use saved hours on more productive work, such as patient care and improving their skills, which accelerates the workflow in the organization, saving thousands annually.
Fewer Errors
Optimized integration of digital tools in the data transmission system enhances the accuracy of transactions by eliminating human intervention, which is prone to mistakes. EDI uses formats complying with predefined standards, which facilitates the completeness of the exchanged information and its validation. In addition, correct details reduce the chances of claim denial and speed up the reimbursement processing.
Compliance and Security
Electronic document exchange follows regulatory protocols such as US law HIPAA (Health Insurance Portability and Accountability Act) for checking patient eligibility to enroll in the health plans. It also ensures the protected transmission and storage of health information to avoid the risk of data breaches.
Better Patient Experience
EDI facilitates cost reduction, time savings, accuracy, and transparency through its real-time communication between concerned parties in the sector. It results in better outcomes, enhanced care quality, and timely resolution of insurance claims for patients, enhancing their overall medical experience.
Why are Healthcare Providers Switching to Automated EDI Solutions?
Healthcare providers, including physicians, pharmacies, insurance companies, and medical labs, are increasingly switching to data exchange automation. The reason is that EDI provides them with enhanced operational efficiency and better profitability due to lower expenses on information exchange and a higher patient satisfaction ratio. Key reasons behind healthcare organizations embracing EDI are listed here:
- The increasing complexity of clinical tasks and growing administrative challenges require an automated platform for seamless data flow between relevant industry partners.
- EDI enhances communication and coordination among different departments and external parties. It reduces the chances of data jams in the system and ensures that the right person gets the important information at the right time.
- Digital integration reduces the functional burden of the units even when there is a growth in their patient volume and associated operations, by providing scalability.
- Standardised document transmission complies with the tight regulations and multiple insurance processes in the healthcare industry, resulting in more innovative ways of information exchange.
Challenges and Limitations of EDI in Healthcare Systems
Electronic data interchange provides several benefits to healthcare providers, but adopting an optimum EDI solution also presents multiple challenges. Despite its perks, the digital tool contains the following limitations:
Integration Complexity
Implementing EDI in an internal setup or electronic medical records is a rigorous process. Different healthcare systems work on distinct platforms, and all the partners may not follow the same formats, creating interoperability issues. Combining them all demands extensive coordination and testing to ensure smooth data exchange.
Upfront Costs
Adopting a new automatic document exchange system includes initial investment in the software, infrastructure, onboarding, and staff training. Even small practices can bring high initial costs and ongoing maintenance expenses, making it difficult for small and medium healthcare institutions to integrate EDI. In addition to navigating the system through evolving state-level standards and HIPAA regulations, continuous audits and tool updates are a must, which eventually leads to more costs.
Change Management
Digital transitions and automation in information exchange may invite staff resistance due to a lack of skills and fear of disruption. Also, an unskilled workforce might not be able to adopt and maintain the electronic system, causing decreased operational efficiency and troubleshooting issues. Furthermore, the new platform must be flexible and scalable to meet the evolving needs of technologies, again putting pressure on staff training.
Best Practices for Implementing EDI Automation in Healthcare
To derive the highest value from the EDI automation in the healthcare industry, organizations should follow the best practices listed below:
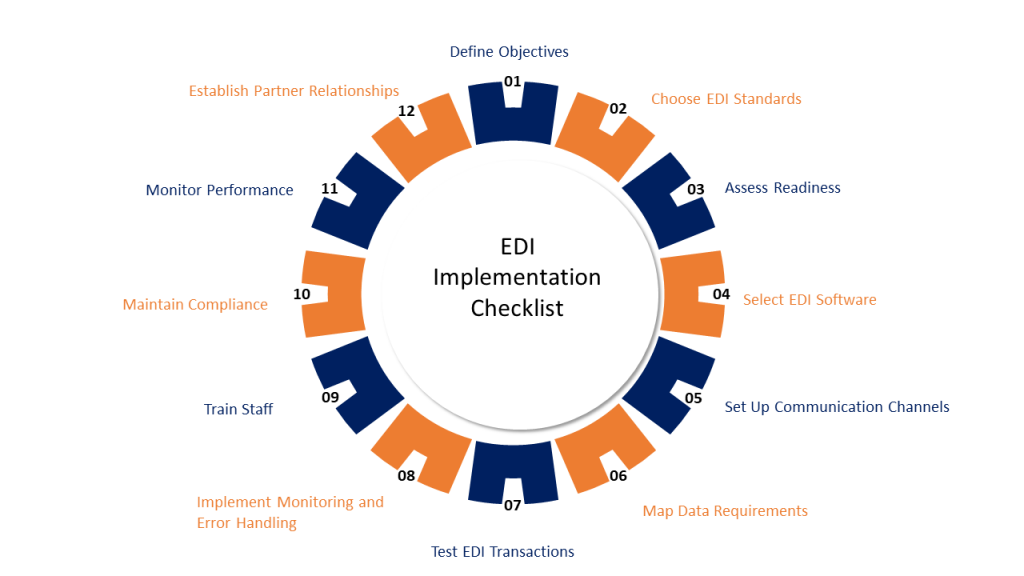
- Investigate the key pain points you want to tackle the most from a technical perspective. The unit can conduct a workflow audit to analyse the current processes and find the major areas requiring digital change. For instance, a patient’s eligibility check may be challenging, and you want to automate it.
- Look for an experienced EDI provider for healthcare transactions who can offer flexibility, scalability, and end-to-end support.
- Go for staff training to educate the team members about the uses of the automated platform and understand its transaction types. Additionally, focus on data quality for successful transmission and accurate results.
- Regularly monitor system performance to address any gaps or potential errors in a timely manner.
Top EDI Healthcare Standards You Need to Know
EDI relies on some specific standards for organised communication, and in the context of healthcare, the following are important ones:
834 (Benefit Enrollment and Maintenance)
Care units enroll eligible patients or staff in health insurance plans through benefit providers, using this standard format. EDI 834 services streamline this process by electronically transmitting enrollment data in a secure and standardized way, ensuring accuracy and compliance with healthcare regulations.
835 (Health Care Claim Payment/Advice)
Insurers use this EDI transaction to send payment details and EOB (Explanation of Benefits) to the healthcare units/hospitals.
837 (Health Care Claim)
The medical center sends it to submit the claim to the insurer/payer via this format directly or through any middleman.
270/271 (Eligibility Inquiry/Response)
Care providers verify patients’ eligibility and benefit coverage by using 270/271.
276/277 (Claim Status Inquiry/Response)
A hospital or medical center tracks the submitted claims and looks over the processes and payment timeline.
278 (Health Care Services Review)
Providers pursue authorization in advance for specific treatment and healthcare services.
820 (Payroll Deducted and Other Group Premium Payment for Insurance Products)
The insurance company processes premium payments on behalf of the medical center.
X12
EDI standardizes transactions between healthcare providers and financial institutions paying insurance, using the American National Standards Institute X12 format.
HL7
Different healthcare application software transmit administrative and clinical data using the HL7 transaction type.
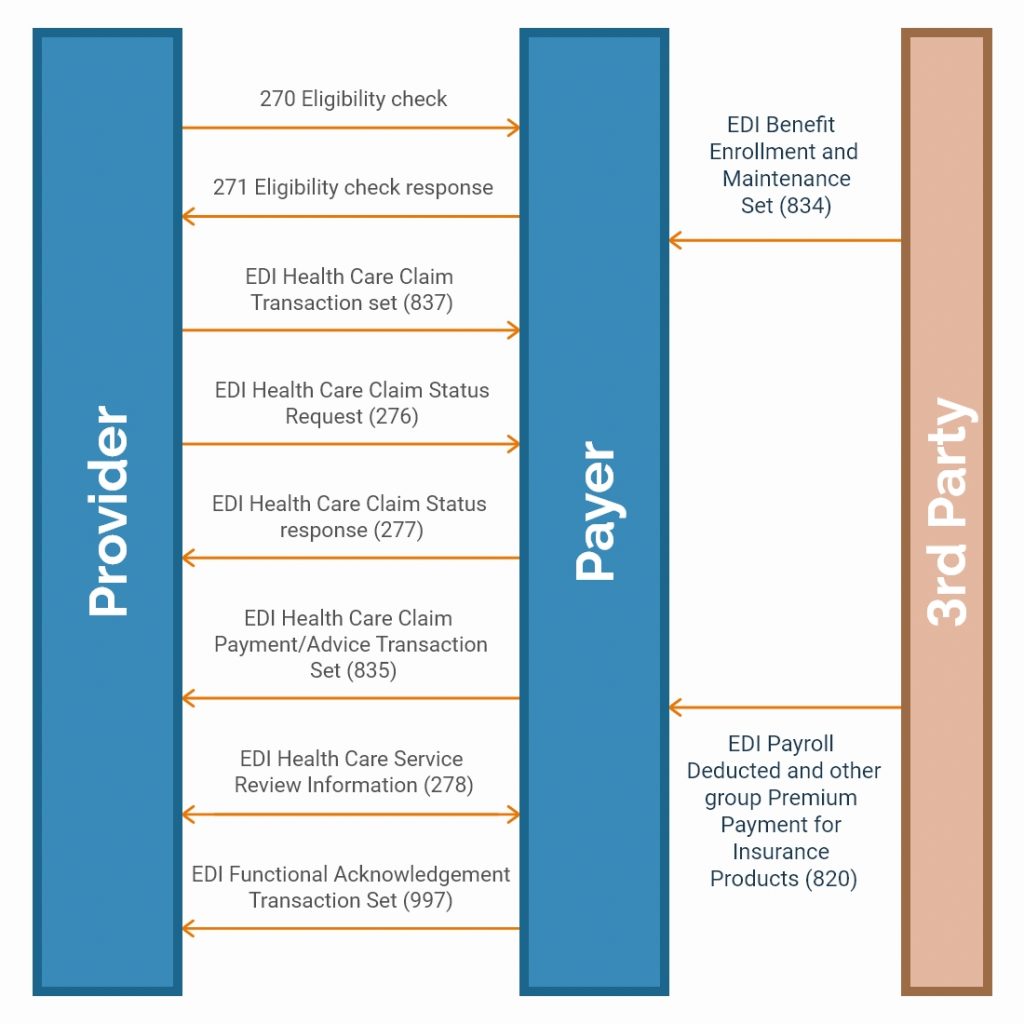
Source:- nalashaahealth.com
Future Trends in Healthcare EDI Automation and Interoperability
- The future of EDI automation and interoperability is embedded in edge computing, cloud-based platforms, and AI integration.
- Healthcare organizations are moving towards a hybrid approach to combine EDI with APIs that can provide greater flexibility.
- Edge computing allows real-time data sharing, minimizing delays in decision-making.
- Machine learning is widely being adopted in the sector for better predictive analytics.
- Cloud-based systems are becoming popular as they reduce IT overheads and offer more flexibility and scalability.
How Can A3Logics Help with EDI Automation In Healthcare?
A3Logics understands the individual challenges faced by healthcare organizations. Our team offers comprehensive EDI solutions to simplify the data exchange like never before and aims to reduce the administrative burden on medical care providers. Whether you aim to streamline your pharmacy coordination or automate claim processing, partner with A3Logics to facilitate EDI automation in healthcare. Our tailored services include:
- Application integration aligns with your unique operational needs.
- Adaptable EDI software that can streamline healthcare transactions without coding.
- Transforms data formats as per specific system and translates into ANSI X.12, TRADACOMS, or EDIFACT standards.
- Provide compliance in data exchange with industry regulations and facilitate audit trails.
- Offer ongoing support and system monitoring for smooth EDI operations.
Final Thoughts
Healthcare transformation in the digital world is progressing, and EDI plays a pivotal role in this journey. Automation is needed at every step, from faster claim processing to timely lab results. In the medical industry, digital data exchange boosts healthcare providers’ competitiveness while making organizations more patient-friendly.
Embracing the electronic documentation system is no longer an avoidable advancement but has become essential for maintaining a quality-driven ecosystem in the sector. With the right EDI partner like A3Logics, caregivers, including hospitals, nursing homes, pharmacies, and insurance companies, can maintain sustainable data sharing operations and deliver superior results.
By implementing electronic document exchange through best practices, clinical institutions can harvest the maximum benefits of the automated system.