Table of Contents
HIPAA 834 transactions are electronic exchanges that allow health plans, providers, employers, and government agencies to share member enrollment data. They help standardize how information about enrollees like names, addresses, coverage details, effective dates, and more is transmitted. The transactions aim to enable the accurate and timely transfer of enrollment data in a secure and interoperable way. This permits healthcare stakeholders to optimize processes that rely on up-to-date member eligibility information.
The HIPAA 834 transaction benefits include lower administrative costs by reducing issues caused by outdated member data. Also, it includes fewer claims’ denials or errors due to incorrect eligibility and better cash flow by promptly resolving eligibility issues.
HIPAA transactions can also help in accurate risk adjustment calculations, payments, analytics and reporting, smoother care coordination, and utilization management.
Here we will provide a comprehensive yet simple overview of HIPAA 834 transactions, its key components and format requirements. Additionally, we will discuss the process for implementing these formats, compliance and security considerations, common challenges that may arise, and potential future trends related to 834 HIPAA transactions. Consult with the top EDI services to ensure HIPAA compliance.
A brief overview of HIPAA and Its Relevance
HIPAA stands for Health Insurance Portability and Accountability Act. It was introduced in 1996 to protect patient’s private medical information. Under HIPAA, doctors, hospitals, and other healthcare providers must keep patients’ medical records and personal information safe and secure. Any organization that deals with patients’ health information must ensure the confidentiality, integrity, and availability of that data.
All patient information like names, social security numbers, medical records, diagnoses, treatments, etc. is considered protected health information under HIPAA. HIPAA sets rules, and guidelines and gives rights to patients regarding their health information. Patients have the right to access their medical records and request amendments if needed. They also have rights regarding how their information is used and disclosed. Overall, HIPAA aims to ensure patients’ trust in the healthcare system by protecting the privacy of their sensitive health information.
Avoid Costly Fines: Ensure Your HIPAA Compliance with Our Solutions
Key Provisions and Objectives of HIPAA
HIPAA or the Health Insurance Portability and Accountability Act, have two main objectives.
- Firstly, it aims to simplify the health insurance administration by standardizing electronic health care transactions. This allows patients to maintain health coverage even if they switch jobs or move to a different state.
- Secondly, HIPAA seeks to protect patients’ personal health information and medical records.
The patients must give consent before information can be shared, with few exceptions. The healthcare providers have to take steps to ensure the security and privacy of patient information. Therefore, strict privacy policies, training employees, and implementing safeguards are required.
Patients are free to report any violations regarding the privacy or security of their health information. The violations of HIPAA rules can result in heavy fines and penalties.
Role of HIPAA 834 transactions in the healthcare industry
HIPAA 834 transaction is used for health plan enrollment and maintenance of member information. It allows health plans to exchange enrollment information electronically with other entities like employers, providers, and government agencies. The transaction also helps reconcile member eligibility data among all parties involved in a patient’s healthcare.
The HIPAA 834 transaction is an important part of HIPAA as it helps standardize and streamline the exchange of enrollment information. It ensures accurate and timely recording of member data which is critical for several purposes:
- Providers need up-to-date eligibility information to verify coverage and HIPAA 834 file claims correctly.
- Health plans need current member data to manage enrollments, process claims and coordinate benefits.
- Employers need accurate enrollment records for payroll deductions, benefits administration, and reporting.
- Government programs like Medicaid and Medicare need correct enrollment data for funding, oversight, and program management.
This transaction plays a vital role in the healthcare industry by facilitating the electronic exchange of member enrollment information between health plans, providers, employers, and government agencies.
Benefits of HIPAA 834 Transactions
HIPAA 834 transactions benefit the healthcare industry in several ways:
- Speed and Efficiency: The electronic exchange of member enrollment data is much faster and more efficient than manual or paper-based processes. It saves time and reduces administrative costs.
- Accuracy: The standardized format of HIPAA 834 transactions helps ensure the accurate and complete transmission of data between trading partners. This helps avoid errors and mismatches in member information.
- Timeliness: Real-time updates of member data through HIPAA 834 transactions help health plans, providers and employers have the most current enrollment information. This is essential for timely claims processing, benefits administration, and performance reporting.
- Security: HIPAA sets security requirements for electronic HIPAA 834 transactions to protect the privacy and integrity of member information. The HIPAA 834 transaction follows standards to ensure only authorized trading partners can access and use the data.
- Compatibility: The standardized format of HIPAA 834 transactions allows data transfer between different systems, software, and health plans. This compatibility and interoperability benefit the entire healthcare industry.
By facilitating the electronic exchange of enrollment data in a secure, accurate, and timely manner, HIPAA 834 transactions help streamline key administrative and business processes across the healthcare system.
Key Components of HIPAA 834 Transactions
A HIPAA 834 transaction has several key components to ensure the accurate and complete exchange of member enrollment information.
- The transaction includes identifying data for both the sender and receiver, along with a document control number for traceability purposes.
- Each member record contains important demographic data like name, date of birth, gender, address, and member IDs assigned by the health plan and employer which helps reconcile information between trading partners.
- Coverage data within each record specifies details about the member’s health plan like the type of coverage selected, effective and termination dates of coverage, subscriber and dependent information, and copay amounts.
- A predesignated segment indicates any special information related to the member’s eligibility or enrollment status.
- An acknowledgment segment verifies that the HIPAA 834 transaction data was received successfully from the sender. Any errors in the transmitted data are also noted here.
These key components ensure that the HIPAA 834 transaction contains all necessary member information to accurately update health plan enrollments, verify coverage and process claims payments between trading partners in a standardized format as defined by HIPAA 834 transaction rules.
The process involved in the HIPAA 834 Transaction
The process involved in HIPAA 834 transactions between trading partners typically includes the following steps.
- The sender first collects enrollment information from employees, members, or other sources that contains member demographics and coverage details.
- The sender then checks the collected data for accuracy, completeness, and compliance with HIPAA 834 transaction format requirements, correcting any errors in the data.
- Next, the validated 834 data is electronically transmitted to the receiver via secure FTP, EDI, or other secure network.
- The receiver acknowledges the successful reception of the HIPAA 834 transactions and notifies the sender of any errors in the transmitted data.
- The receiver then loads the valid HIPAA 834 transaction data into its system and updates member enrollment records accordingly.
- Any changes to member coverage or eligibility that occur after the initial 834 transmissions are then notified to the trading partner via periodic HIPAA 834 transaction updates sent by the sender.
- The trading partners regularly reconcile their enrollment data to identify and resolve any mismatches ensuring data accuracy between both parties.
By following this process, trading partners can effectively use HIPAA 834 transactions to continually maintain accurate member enrollment information in a secure, timely, and HIPAA-compliant manner. The focus is on maintaining data accuracy and compliance while enabling the efficient and real-time exchange of enrollment information critical for proper health plan administration and claims processing.
Consult about HIPAA 834 Transactions
Meet Our EDI experts that will guide you through the complete process of HIPAA EDI 834 transactions
Issues and challenges faced during HIPAA 834 transactions
While HIPAA 834 transactions aim to standardize and streamline member enrollment data exchange, there are still some issues and challenges faced during implementation:
- Data quality: Incomplete or inaccurate enrollment data submitted in 834 HIPAA transactions can lead to problems like delayed claims processing, incorrect benefits, and coverage errors. Thorough data validation is required.
- Compatibility: Different systems, formats, and versions used by trading partners can cause compatibility issues during the HIPAA 834 transaction data exchange. Proper testing and certification are needed.
- Connectivity: Network connectivity and reliability are critical for the timely submission and reception of 834 transactions. Downtime and delay can impact processes.
- HIPAA 834 transaction Errors: Errors in HIPAA 834 transactions during submission or loading can disrupt business processes till issues are resolved. Thorough error tracking and correction are required.
- Security: Ensuring the security of member information during electronic data exchange as required by HIPAA is an ongoing challenge. The latest security technologies need to be implemented and updated regularly.
- Resources: Proper resources, staff training, and technical expertise are required to effectively manage and gain full benefits from HIPAA 834 transactions. Many organizations still face resource constraints.
While electronic enrollment data exchange using HIPAA 834 transactions offers many benefits, healthcare organizations need to address these challenges to implement and maintain successful HIPAA compliance.
Compliance and Security Considerations in HIPAA 834 Transactions
HIPAA 834 transactions must comply with HIPAA Security and Privacy Rules to securely exchange protected health information electronically. Healthcare organizations need to implement appropriate administrative, physical, and technical safeguards to comply with HIPAA 834 transaction security requirements for electronic transactions. This includes:
- Assigning security officials and designating security personnel roles.
- Implementing access controls like unique user IDs and passwords.
- Conduct risk analyses and risk management plans.
- Encrypting electronic protected health information during transmission and storage.
- Controlling access to workstations and devices used for HIPAA 834 transactions.
- Strictly segregating duties to limit access on a need-to-know basis.
- Implementing intrusion detection and firewall systems.
- Conduct regular security audits and assessments.
- Providing security awareness training to all personnel handling electronic transactions.
- Establishing response plans for security incidents and handling security breaches properly.
Failure to comply with HIPAA 834 transaction security requirements for HIPAA 834 transactions can result in loss of member data privacy, data corruption, business disruption, fines, and penalties, and loss of patient trust. Healthcare organizations need to give security the highest priority.
Industry Standards and Implementation Guides
Healthcare organizations must follow certain industry standards and implementation guides to correctly format and exchange enrollment data using HIPAA 834 transactions. The key standards and guides that govern HIPAA 834 transactions are:
- The ASC X12N 834 Benefit Enrollment and Maintenance standard. It defines the content, structure, and syntax for 834 transactions.
- ASC X12N 005010X220 Implementation Guide. It provides more details on how to implement the 834 standard, including data element specifications.
- The National Council for Prescription Drug Programs (NCPDP) guides pharmacy-related 834 transactions.
- Centers for Medicare and Medicaid Services (CMS) guides 834 HIPAA transactions related to government health programs.
Trading partners must adhere to the same implementation guides to ensure the interoperability and compatibility of HIPAA 834 transactions. Guides are periodically updated to accommodate changes in standards, regulations, and industry needs. Healthcare organizations need to have processes in place to regularly update their systems and ensure ongoing HIPAA compliance as guides evolve. Strict adherence to current industry standards and implementation guides is essential for the accurate and secure exchange of member enrollment data using HIPAA 834 transactions.
HIPAA 834 transaction Formats
HIPAA 834 transactions use electronic data interchange (EDI) formats to exchange member enrollment data between trading partners. Two common EDI formats are used for 834 transactions by EDI 834 services providers:
- Flat HIPAA 834 file Format – A simple text-based format where data elements are separated by delimiters like commas, tabs, etc. This is an easy format to implement but offers less error-checking.
- XML Format – Data is tagged and structured using XML. This format provides more data validation and is more readable. However, it requires XML parsing.
The specific EDI format used for a HIPAA 834 transaction depends on the requirements and capabilities of the trading partners. Both flat file and XML formats are compliant with HIPAA standards.
Some key considerations when choosing a format are:
- Compatibility with trading partners’ systems
- Ability to meet data validation and security needs
- Cost and resources required for implementation
- Ease of data integration and error correction
- Flexibility to adapt to future changes
HIPAA 834 enrollment data can be exchanged using either flat file or XML formats, as long as the specific requirements for each data element are met according to the related implementation guides. The chosen format should match the needs of all involved trading partners.
Benefits of integrating HIPAA 834 transactions with other systems
Integrating HIPAA 834 transactions with other key systems can bring many benefits to healthcare organizations:
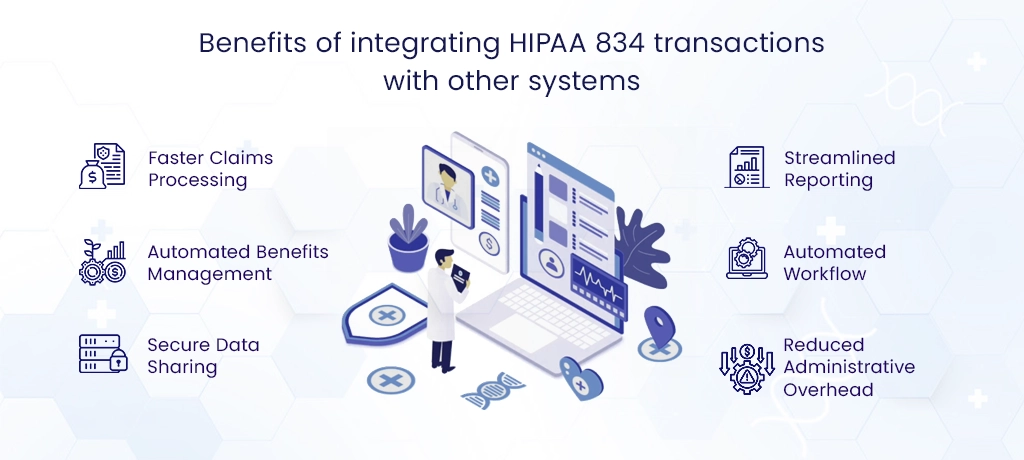
- Faster Claims Processing: When HIPAA 834 transaction data is loaded directly into claims processing systems, it ensures accurate and timely member eligibility verification during claims adjudication. This speeds up reimbursement.
- Automated Benefits Management: HIPAA 834 transaction integration with benefits administration systems helps automate processes like eligibility checking, premium billing, and payroll deductions. This reduces manual work and errors.
- Secure Data Sharing: Integrating HIPAA 834 transactions with electronic health record (EHR) and patient portal systems allows secure, real-time access to updated member enrollment data. This helps provide appropriate care and services.
- Streamlined Reporting: The integration of HIPAA 834 transaction data with reporting and business intelligence tools helps generate accurate and timely reports on performance metrics, revenue cycle management, and regulatory compliance.
- Automated Workflow: Connecting HIPAA 834 transaction information with workflow management software can automate tasks like notifying providers of member eligibility changes or sending coverage verification requests to employers.
- Reduced Administrative Overhead: Overall, integrating HIPAA 834 transactions with key healthcare IT systems can reduce administrative workload, eliminate redundant data entry and minimize issues related to outdated or inaccurate member information.
Impact of HIPAA 834 Transactions on Healthcare Organizations
HIPAA 834 transactions have a significant impact on the functioning and performance of healthcare organizations:
Health plans – Timely and accurate member enrollment data received through HIPAA 834 transactions helps ensure:
- Correct claims adjudication and payment to providers
- Proper calculation and collection of premiums from employers and members
- Appropriate risk adjustment and revenue allocation
- Accurate enrollment and dis-enrollment reporting to Medicare and Medicaid
For employers – The ability to electronically send group health plan enrollment data to insurers via HIPAA 834 transactions helps:
- Reduce administrative workload related to benefits management
- Ensure correct premium billing and payroll deductions for employees
- Resolve eligibility issues promptly
- Prepare reports on healthcare spending and utilization for employees
For providers, – Reliable member eligibility information received through HIPAA 834 transactions enables the following:
- Correct eligibility verification at the time of service
- Accurate claims submission with appropriate member IDs
- Timely collection from health plans and members
- Reduction in denials and revenue leakage
Focus on Your Patients, Not Paperwork: Get Expert Help with HIPAA Compliance
Future Trends and Developments
Several trends and developments are likely to shape the future of HIPAA 834 transactions:
- Move to Real-time Data Exchange: More organizations are moving from periodic HIPAA 834 transaction data submissions to real-time or near real-time exchange of enrollment changes. This ensures the most up-to-date eligibility information.
- Integration with EHRs and Care Management Systems: Better integration of HIPAA 834 transactions with electronic health record systems and care management tools can improve the coordination of care and population health management efforts.
- Use of APIs and Cloud Technologies: The use of APIs (application programming interfaces) and cloud-based EDI solutions may simplify and streamline the HIPAA 834 transaction process, making it more accessible to smaller providers and practices.
- Adoption of FHIR Standards: The use of FHIR (Fast Healthcare Interoperability Resources), an emerging data standard for health information exchange, may replace current formats for 834 HIPAA transactions in the future.
- Expansion to Non-Medical Data: HIPAA 834 transactions may start including more social determinants of health data in addition to traditional medical and eligibility information.
- Focus on Data Quality: With value-based payment models gaining prominence, there will be more focus on using high-quality HIPAA 834 transaction data to improve risk adjustment calculations, care management, and clinical outcomes.
Conclusion
HIPAA 834 transactions play an important role in the healthcare system by facilitating the electronic exchange of member enrollment data between health plans, providers, employers, and government agencies. The standardized format and processes defined for HIPAA 834 transactions help make this data exchange accurate, secure, and efficient.
However, ensuring compliance with HIPAA rules, maintaining data quality, and addressing issues like system compatibility remain ongoing challenges for organizations implementing 834 transactions. With technology advancements and industry demands evolving rapidly, the future of HIPAA 834 transactions is likely to see developments like real-time data exchange, integration with other healthcare IT systems, and adoption of new data standards.
Overall, efforts to improve HIPAA 834 processes have the potential to enhance core administrative functions, care coordination, population health management, and value-based care.